tomos123
Pneumococcal Sepsis in a Patient with Asplenia and Hypogammaglobulinemia ( 2 фото )

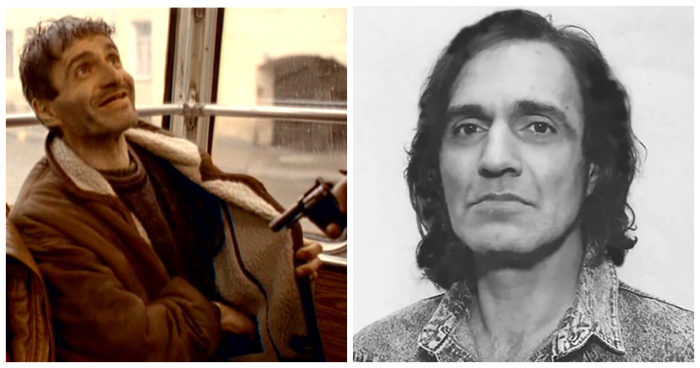
A 52-year-old man with a history of traumatic splenectomy and treated mantle-cell lymphoma presented with a 5-day history of dry cough and nasal congestion and a 2-day history of dyspnea and confusion. Three years earlier, the lymphoma had been treated with chimeric antigen receptor (CAR) T-cell therapy. The lymphoma had been complicated by persistent hypogammaglobulinemia, for which intermittent immune globulin infusions had been given. The patient had had appropriate pneumococcal vaccinations and had received penicillin prophylaxis for 12 months after CAR T-cell therapy. At the current presentation, his body temperature was 102.7°F (39.3°C), heart rate 128 beats per minute, blood pressure 78/48 mm Hg, and oxygen saturation 84% while he was breathing 6 liters of oxygen by nasal cannula. Physical examination was notable for coarse breath sounds and cyanosis of the hands and feet. A chest radiograph showed multifocal consolidations. Computed tomography of the head showed maxillary sinusitis. The patient was admitted to the intensive care unit. Serum immunoglobulin levels were undetectable. Blood cultures grew Streptococcus pneumoniae 7 hours after collection. Encapsulated diplococci were seen in 20% of neutrophils on a peripheral-blood smear (Panel A, Wright’s stain). A diagnosis of septic shock from invasive pneumococcal infection was made. Multiorgan dysfunction and purpura fulminans of the nose (Panel B) and fingers (Panel C) developed. On hospital day 8, the patient died.
Samuel J. Starke, M.D. , and Ira Miller, M.D.
Published October 11, 2025
N Engl J Med 2025;393:1521
DOI: 10.1056/NEJMicm2505757
VOL. 393 NO. 15

Крепкого здоровья!
Взято: Тут
1777